Supporting Health-Care Financing Reform in Mongolia: Experiences, Lessons Learned, and Future Directions

Enjoy the tour of two community care centers ADB help renovate and refurbish. The centers are a part of ADB’s Yichang Elderly Care Demonstration Project.
Related event: Elderly Care System Development Forum
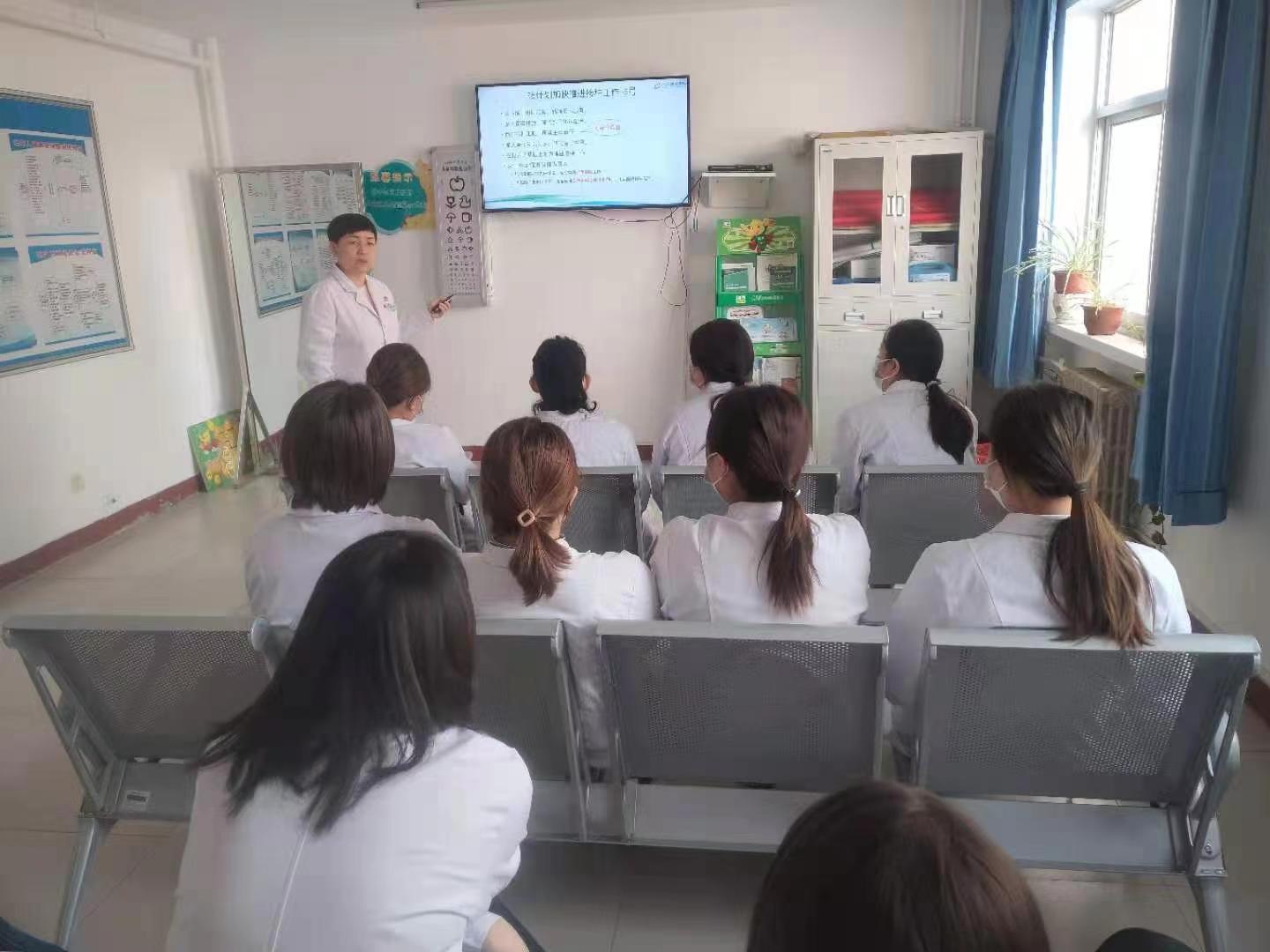
What is the role played by the Yichang Elderly Care Demonstration Project’s management office staff? What challenges do they face? Listen to how the Yichang project strengthen their capacity.
Related event: Elderly Care System Development Forum

Watch how ADB financing for Hubei Three Gorges Polytechnic help establish a high-quality elderly care curriculum.
Related event: Elderly Care System Development Forum
Watch key moments in project programming, appraisal, identification, and implementation of ADB’s Yichang Elderly Care Demonstration Project. Listen to some of the difficulties encountered, and solutions as well as innovations introduced.
Related event: Elderly Care System Development Forum


The coronavirus disease (COVID-19) swept across the world in early 2020, upending economies and bringing misery to millions. By 2022, the disease had started waning, if unevenly. In many countries, people started going about their business unmasked; in others, they kept their masks on and their distance from each other.
The pandemic didn’t subside on its own. A global effort to prevent the spread of the disease, develop vaccines, and vaccinate most of the world’s population slowed the virus. But variants—some more lethal than others—are discovered regularly and public health authorities remain vigilant. The pandemic is not yet a distant memory.
In the PRC—ground zero for the pandemic and with the biggest population in the world—the stakes were and continue to be especially high.
News of the first infections, in Wuhan, Hubei, broke in late January 2020, on the eve of Chinese New Year. Little was known of the virus except that it was new, that it spread quickly, and that people had already died from it.
Health-care workers and volunteers from across the PRC joined the battle against the disease. Six shared their stories. They include doctors and nurses, seasoned and less so, and a young man with no medical training and nothing but enthusiasm.
Three work in Litong District, Wuzhong (population 1.4 million), Ningxia Autonomous Region, north-central PRC. Lina Wang is a health-care worker at Shengli Township Community Health Service Center. Yanfang Li is director of Jinxing Garden Community Health Service Station. And Dr. Lianzhi Zhang came out of retirement and moved from Hefei City to work at the Shengli center.
Two of the interviewed frontliners are from Heifei (population 5 million), Anhui, in eastern PRC. Dr. Hua Niu is a chief physician at Anhui Provincial Chest Hospital. A veteran of the battle against severe acute respiratory syndrome (SARS), she was one of the first health workers to troop to Wuhan. Dr. Yin Liu is a member of the health education unit of the provincial Center for Disease Control. He, too, was sent to Wuhan.
Jin Chen, a young man working in clothing retail in Wuhan, offered invaluable logistical and moral support to the frontliners.
Most left their homes for weeks and all risked their health to hold the line against the virus. They will not soon forget how hard it was to be away from family, the crushing hours, and the mental and emotional toll on themselves and others. They all overcame fear and exhaustion to get the job done. None regretted the experience.

Interviewer and Public Health Specialist (Consultant)

Translator and Researcher (Consultant)


While the world was trying to grasp what had hit it in early 2020, the still-mysterious coronavirus disease (COVID-19) wasn’t the only thing that made life hard for Yanfang Li, 45. Sometimes it was the people she and her colleagues were caring for.
A nurse, she’s the director of Jinxing Garden Community Health Service Station, Litong District, Wuzhong City, Ningxia Autonomous Region. She’s worked there for 14 years with 2 physicians, 12 nurses, and 2 other staff members. It’s 1 of 13 stations under the Shengli Township Community Health Service Center, Litong.
COVID-19 wasn’t the only thing that made life hard for Yanfang Li. Sometimes it was the people she and her colleagues were caring for.
News of the pandemic filled Director Li with dread. But after station staff received personal protective equipment and started monitoring people under home quarantine and teaching them how to prevent spreading COVID-19, the fog of uncertainty began to lift.
Not everyone was grateful. “In Chongyan neighborhood,” she recalled, “a family yelled at staff, making them cry in anger. The police hadn’t yet started compelling residents to comply with health protocols.” The station called on the neighborhood committee for help. Even then, she said, “Sometimes residents didn’t take our calls. Sometimes they shouted at us.”
“Some who did take our calls said they weren’t getting any help,” she said, “that no one was listening to them, that they were panicking. Some worried they had COVID-19, so we got them to the city hospital for X-rays. We didn’t have nucleic acid tests yet, but at least we could counsel them.”
Residents might have been stubborn because they were frustrated and afraid…. Psychological counselling is just as important as treating the disease.
A case has stuck with Director Li because it underscored the importance of counselling. A man working in Wuhan had returned to Jiexin neighborhood for Chinese New Year. His colleagues turned out to be infected. He quarantined at his girlfriend’s home and, although he had no symptoms and had his own room and bathroom, he was terrified he would infect the household. With a grid worker, Director Li and a station physician, Dr. Yang, comforted him in person and through WeChat. “We eventually sent him for an X-ray—he wasn’t infected,” she said. “He was so relieved and grateful.”

“Things started calming down in the spring of 2021, when nucleic acid testing started,” Director Li said, “and in mid-2021, when vaccination started.” By August, health personnel had tested the city’s 1.4 million people. Then someone with COVID-19 returned from Inner Mongolia, sparking an outbreak. The whole city had to be retested in August and September.
“We got home after 8 or 9 at night, slept, and did it all over again the next day starting at 6. All grassroots frontliners, old and young, with or without children, went all out.”
“We worked with the neighborhood committees and with Wuzhong City Hospital professionals,” Director Li recalled, “and collected samples every day, including from the quarantined and bedridden. We couldn’t go home for lunch. Take-away restaurants were closed. The township health center leader gave us instant noodles and ‘self-heating’ rice. We got home after 8 or 9, slept, and did it all over again the next day starting at 6. All grassroots frontliners, old and young, with or without children, went all out.” Even young nurses with babies. “Two had to stop breastfeeding,” she said. “The children’s grandparents stepped in to help.”
“When vaccines first became available,” she said, “residents were eager to be vaccinated, but supply was tight. Some lined up for hours, starting at 3 or 4 in the morning. But when we finally had enough vaccines, some people worried about side effects. We worked with the neighborhood committees to change their minds.”
“You must be organized to do a good job. Staff must be skilled, fast, and accurate. They must interact with and organize residents with the help of neighborhood committees.”
In the evenings, Director Li planned how best to avoid chaos at the vaccination sites. “I used to have trouble sleeping when my supervisor thought I didn’t do well,” she said, adding proudly, “but Wuzhong responded swiftly and the measures we’re taking are the best.”
Still, she said, “I am most worried about the virus spreading because everything is so closely linked. The last thing we want is big outbreaks as in Wuhan and Xi’an.” Wuzhong had a close call in October 2021, she said. A bus driver was taking eight tourists back to the city from Inner Mongolia, heard that COVID-19 had broken out there, and brought them directly to Wuzhong City Hospital for testing. All except the quick-thinking driver were positive and immediately quarantined.
Director Li cannot stress enough how important it is to stick to standardized procedures. “We must be organized,” she said. “Staff must be skilled, fast, and accurate. They must interact with residents with the help of neighborhood committees.”
“We shouldn’t wear down our grassroots staff, who are so underpaid. Planning must be based on sound analysis.”
“And,” she cautioned, “we shouldn’t wear down grassroots staff, who are so underpaid. Planning must be based on sound analysis. Some leaders play it safe and delegate everything. Or they overreact with lockdowns and mass testing.”
After an extraordinary 2 years of battling the pandemic, Director Li is still moved by the staff’s dedication—how they never complained no matter how drained they were and how they ran courageously to the front. “One night,” she recalled, “I phoned four staff for emergency test sample collection. They all arrived on time. No excuses, not even from those who had to leave their babies. They were ready to go. I was so proud of them.”

Interviewer and Public Health Specialist (Consultant)

Translator and Researcher (Consultant)


On 15 February 2020, Dr. Yin Liu, 33, arrived in Wuhan City with a team sent by the Anhui provincial Center for Disease Control (CDC). His wife found out only the next day, from watching the news. When she called to ask why he hadn’t told her, he said the epidemic was serious and he didn’t want her to worry; she had her hands full enough with their 13-month-old son. They kept in touch on WeChat every night. He asked her not to tell his aging parents.
Dr. Liu has worked in the health education unit of the provincial CDC in Hefei City, Anhui Province for 6 years with four others. Before the COVID-19 pandemic, he had majored in medicine and then worked on health literacy for 6 years.
The CDC sent 13 people to Hubei Province in three batches. Dr. Liu was in the second one. He stayed for 44 days, until the end of March. “Not many people were sent to the frontline,” he said. “It was unforgettable.”

Before he left for Wuhan, CDC staff were monitoring Wuhan. By the eve of Chinese New Year, they were on edge. The CDC leadership worked through the holiday. “I was at home,” Dr. Liu recalled, “but told the leaders that if they needed me to fight the epidemic, I would return to work immediately. My colleagues and I wouldn’t hesitate. It’s what we were trained for. We were on 24-hour stand-by.”
With the confidence of youth, Dr. Liu said, “I wasn’t afraid of being infected as long as we protected ourselves. And if I did get infected, the worst that could happen would be a mild case.”
What they saw in Wuhan, however, alarmed them. The CDC had sent the teams off with all its N95 face masks and enough personal protective equipment (PPE). “But we found that health professionals in Wuhan had been infected because they didn’t have enough PPE,” Dr. Liu said. “Some wore the same face masks for days. One staff member of the district CDC where we worked became infected after we arrived. Luckily, it was a mild case and she recovered and returned to work with us. She was really dedicated.”
The uncertainty and long hours were hard on Dr. Liu and his colleagues. They still didn’t know what they were dealing with. Dr. Liu’s team had never even had to deal with infectious disease control. They fast-tracked learning epidemiological investigation from an older, experienced colleague. They practiced calling close contacts and became more confident. The first 2 weeks were hectic, then the team got into the swing of things.
Still, Dr. Liu said, “We were anxious, worried. We were staying at the quarantine hotel and wore two face masks when we went out. It was freezing. Everyone caught cold. I did twice. We hadn’t brought enough cold medicine and couldn’t get it in Wuhan during the strict lockdown. We had to share whatever we had. Later, the Anhui CDC sent us medicine, clothes for warmer weather, instant noodles, and the like, and things got better.”
Dr. Liu and his colleagues couldn’t go out after work to take their mind off things. After dinner, they gathered in the corridor of the hotel, masked and at a safe distance from each other, to chat, smoke, tell jokes, and laugh.
“A challenge,” he said, “was worrying about my family back home. They fully supported what I was doing. But how would they cope? We eventually told my parents I was in Wuhan. My mother moved to Anhui to help my wife look after our son. My wife couldn’t go to work because of the pandemic. I missed them a lot.”
Dr. Liu had some words of encouragement for less experienced health workers. “When we were first sent to Wuhan,” he said, “we had to learn quickly on the job. We learned from doing.” As for the future, he stresses that everyone must be prepared. “A lot of provincial CDC staff are recent graduates,” he said. “We’ve suggested that all CDC personnel learn basics skills such as simple PCR sample collection by performing the procedure on each other. That way, when a new epidemic occurs, everyone from the CDC can get hands on and help right away.”

Interviewer and Public Health Specialist (Consultant)

Translator and Researcher (Consultant)


“Of course, you can’t just stay home. You have to help,” Jin Chen’s mother told him over dinner in February 2020. Wuhan had just been locked down because of COVID-19 and health workers from all over the country were descending on the city, which was ground zero for the disease.
Before the pandemic, Mr. Chen had been working in clothing retail in Wuhan for more than 10 years. It soon became clear he wouldn’t be returning to work any time soon. His family has always believed in giving back through volunteer work, and he scanned WeChat to see what he could do. “The government was recruiting volunteers and I signed up,” he said.
Mr. Chen made his mother promise not to tell family members because he didn’t want them to worry. “Somehow,” he said, “my cousin found out. His wife worked in a hospital that gave out personal protective equipment (PPE). He sent me some, including face masks, goggles, gloves, and more than 10 sets of protective clothes and told me to call if I needed more. Volunteers received our own PPE from the government, but what my cousin did was so heartening.”
“My first task was to go to the airport to greet the health workers coming from all over the PRC,” he said. “My fellow volunteers and I took them to their hotels and workstations and helped them settle in. After a few days, I became a health station leader at a hotel, which meant staying there full-time. It was hard to say goodbye to my mom. We cried. We didn’t know how long I would be there or whether I would even return home safe and healthy.”
Mr. Chen worked at the hotel in Wuchang District from 23 February to 31 March. That’s where he met Dr. Yin Liu of the Anhui provincial Center for Disease Control, who had arrived a week earlier. Twenty-three other health workers had come from Anhui, Henan, and Maanshan.
“I was the main contact point and liaison between the visiting health workers and the partners in Wuhan—the local government, the community, and health services, including the Wuchang district Center for Disease Control and Prevention,” he said. “I worked closely with all of them almost 24/7 to ensure everything was all right—accommodation, food, transport, access to services, and so on. In the evening, I took their orders for breakfast—some wanted noodles, others porridge, with different flavors or time of delivery—and told the cafeteria that was supplying us. We had to make sure the hotel rooms were heated well and that the health workers could reach their destinations on time to do their epidemiological investigation or polymerase chain reaction (PCR) test sample collection and other tasks.”
“We were so grateful to the government and others who supported us,” he said. “We didn’t have our own vehicles and other provisions. They supplied them, bringing us to where we needed to go. I learned about disinfection, what contaminated and semi-contaminated areas are, how to wear PPE properly, and lots of medical terminology and skills. I was so impressed by the health workers’ dedication and professionalism.”
Dr. Liu praised the volunteers for making the health workers feel welcome. “Mr. Chen,” he said, “bonded with us and we worked closely for about 40 unforgettable days. He wept when he saw us off at the airport at the end of March. He stays in touch with some of us. My colleagues and I wrote him an official letter expressing our gratitude for his dedication.”
“We did our best,” Mr. Chen said. “Some of the health workers caught cold and some felt anxious, especially at the beginning when so little was known about the virus. We comforted them, especially the newly arrived ones, when they felt down, sleepless, or homesick. We helped them get PCR tests when they felt unwell. I bought birthday cakes and organized birthday parties for some—with social distancing—and brought them chang shou mian or longevity noodles. Sometimes we asked people in the neighborhood to bring them re gan mian—the ‘hot dry noodles’ that are a Wuhan specialty—as a treat. We wanted the health workers to know we cared about their well-being.”
Despite taking all precautions, however, Mr. Chen had a scare. A grocery store thermometer showed his temperature at over 37.3°C. He holed up in his room for 3 days, doing his work over the phone and WeChat. He emerged from isolation when he felt better. It turned out it was nothing serious. “Everyone laughed at me,” he said. “That was the only time I was really frightened. But as long as you take preventive measures, you shouldn’t be afraid, even of omicron.”
Mr. Chen knew the risk but that didn’t stop him from volunteering. “My mom often told me the health workers were so brave and selfless for coming to Wuhan to help us,” he said. “We couldn’t stay idle! That’s what I was most proud of doing for my city. It made me feel better than a billion yuan ever could. And my mom is so proud of me.”

Interviewer and Public Health Specialist (Consultant)

Translator and Researcher (Consultant)

“We were like soldiers,” Dr. Hua Niu said. “We wore uniforms and armbands and followed orders.” She was one of thousands of health-care professionals from all over the PRC who trooped to Wuhan, Hubei Province to help fight an emerging and quickly spreading virus in February 2020. The city was ground zero for the coronavirus disease (COVID-19) pandemic.
Now a chief physician at Anhui Provincial Chest Hospital, where she has worked for 20 years, Dr. Niu, 42, specializes in respiratory and critical disease treatment, overseeing 18 staff. The imposing hospital has 1,300 beds, 26 clinical departments, and 827 health-care professionals. It’s in Heifei (population 7.5 million), the capital city of Anhui Province (population 64 million), eastern PRC.
After news of the pandemic broke, the hospital, a 5-hour drive from Wuhan, was on high alert, with continuous, tense text messages flooding hundreds of phones.
After news of the pandemic broke, her hospital, a 5-hour drive from Wuhan, was on high alert, with continuous, tense text messages flooding hundreds of phones. Any news, official or unofficial, put staff on edge, especially when they heard that health-care workers in Wuhan lacked personal protective equipment (PPE) and supplies.
A veteran of the battle on two fronts against the 2003 severe acute respiratory syndrome (SARS), Dr. Niu faced the still-unknown disease more calmly than most. She was part of the seventh medical team from Anhui and the third from her hospital to be sent to aid Wuhan. “By then,” she said, “the PPE shortage had eased somewhat. We each received a big suitcase for PPE, personal daily needs, backup medicine, and so on.”
While she wasn’t anxious about traveling to Wuhan, however, she had her family to deal with. She’s an only child, her daughter was only 8 at the time, and her husband was an extremely busy surgeon. Her grandmother was living with them, bedridden because of a stroke and suffering a high fever. Wuhan was already in lockdown, and all over the country people with fever were being treated with caution; Dr. Niu’s grandmother couldn’t go to the clinic or hospital. Dr. Niu cared for her at first, bringing home infusion liquid, unsure that her fever could be controlled. The grandmother was eventually admitted to Dr. Niu’s hospital, where family could visit her.
Dr. Niu’s team worked with other medical teams from all over the PRC to help Wuhan in the war against the unprecedented outbreak.
Dr. Niu’s team worked with other medical teams from all over the PRC to help Wuhan in the war against the unprecedented outbreak. For 34 days, they worked long hours in Wuhan Central Hospital, which had redesigned its wards for COVID-19 patients. A few minutes away from the hospital is the wet market from which the virus had spread.
Health-care professionals of the hospital had been infected. Some died. Their photos hung on corridor walls were a somber reminder of what was at stake.
The hospital was where Dr. Li Wenliang had worked. An eye doctor, he died on 7 February 2020, less than 2 weeks before Dr. Niu and her colleagues arrived, after contracting what he had tried to warn his colleagues was a new SARS-like disease. Other hospital health-care professionals had also been infected. Some died. Their photos hung on corridor walls and in the buffer area, where Dr. Niu and her colleagues changed their clothes, a somber reminder of what was at stake.
Some local staff were their patients. A nurse whose wife had recently given birth and who had not seen the baby yet. A chief physician from the nephrology department. Seeing the hospital staff’s suffering was hard on Dr. Niu and her team.
She was the deputy group leader of the COVID-19 critical care group in the seventh medical team, composed of about 170 health professionals and fewer than 10 associate chief physicians. She led one of the six critical care groups.
She walked briskly through the isolation ward the first time she and a deputy director made the rounds. Other staff told her to slow down because they feared that raising the dust on the floor would spread the virus. “I had worked in isolation wards,” she said, “including during the SARS outbreak, so I wasn’t worried. But some doctors were jumpy.”
 Dr. Niu making the rounds of COVID-19 patients.
Dr. Niu making the rounds of COVID-19 patients.
The staff worked in three 8-hour shifts, taking 2 hours to get from their apartments to the wards. Public buses were turned into shuttles for health professionals. They had to be in the bus 30 minutes before departure, spent an hour on the road, and took another 30 minutes to disinfect and get into their PPE. After their shift, they had to go through the reverse process, getting home 2 hours later.
Caring for the elderly was especially hard. “Family members and private caregivers were barred from the wards,” Dr. Niu said. “And the nurses were overworked. Sometimes an elderly patient would fall and break a bone. We could only take X-rays and send them to specialists, who helped assess and diagnose patients remotely. We had to deal with family members by phone.”
Dr. Niu ate only twice a day. “I didn’t drink anything at the hospital,” she said. “We didn’t eat anything, either, although the hospital provided lunch boxes. We didn’t want to take our face masks off.” She developed stomach trouble and, not long after returning to Anhui, had to have a gastroscopy.
Staff endured other aggravations. “I wore diapers so I wouldn’t need to go to the toilet,” she said. “We stood in line to go to the toilet and to shower after our shift. We had to exchange shifts so that menstruating nurses and doctors could take time off. But we managed.”
She was exhausted. “Even after work,” she said, “I had to communicate with patients’ families and the hospital, using my own phone. Some patients had had strokes, some had diabetes, some were on dialysis. We couldn’t conduct face-to-face multidisciplinary medical consultation. But we just got on with it.”

Dr. Niu in her scrubs: She and her colleagues from Anhui kept up their spirits while battling the COVID-19 outbreak in Wuhan in February 2020.
Although Dr. Niu was more seasoned than many of her colleagues, the work started to get to her. “The night shift could be hard,” she said. “I couldn’t sleep well during the day. My apartment was near an overpass. There wasn’t much traffic—just trucks, some ambulances—but it was noisy. My ears started ringing.”
Some health-care workers needed comforting. “Some of us were senior and experienced,” she said, “but we had a young nurse—the only health-care worker sent from a hospital in Tongling—who became nauseous and had cold-like symptoms. Our team’s head nurse wanted to give her some medicine. The young nurse was frightened and told her not to come near and to leave it at the door. The young nurse described her symptoms to me over the phone. She was in a near panic but I didn’t think it was COVID-19 and tried to soothe her. We shared the medicine we had brought from Anhui with her and she felt better after 2 days.”
Dr. Niu and her colleagues managed to keep up their spirits. “Eleven of us from Anhui lived in separate rooms in the same apartment building,” she said. “We weren’t allowed to visit each other but we could stand in our doorways and chat. When we distributed supplies, we could catch up and socialize.”
It helped that her family was fine. “They weren’t that worried,” she said. “My grandmother was often in tears, but my parents were looking after her. My mother-in-law helped look after my daughter. My husband checked her homework. The child was a welcome distraction for everyone. I had a phone or video call with the family almost every day.”
“When we notice something extraordinary or suspicious, such as rare diseases, we have to tell our superiors. Nipping the problem in the bud is more effective than containing it after it’s spread.”
“We need to be meticulous,” Dr. Niu said, reflecting on what should be done to prevent another pandemic. “When we notice something extraordinary or suspicious, such as rare diseases, we have to tell our superiors. Nipping the problem in the bud is more effective than containing it after it’s spread.”
“Female comrades have physical issues, have young kids. But at the height of the pandemic, they overcame all challenges. I think human capacity to endure is almost limitless.”
Women, she noted, have a double burden. “If tasks cannot be completed within working hours,” Dr. Niu said, “we need to work overtime. Many become hoarse, like me, or sick. After work, there’s housework. I take care of things at home. I go to sleep late. It’s either be more efficient at work and at home or else stay up at night.”
“Female comrades have physical issues, have young kids,” she said. “But at the height of the pandemic, they overcame all challenges. I think human capacity to endure is almost limitless.”

Interviewer and Public Health Specialist (Consultant)

Translator and Researcher (Consultant)
© 2026 Regional Knowledge Sharing Initiative. The views expressed on this website are those of the authors and presenters and do not necessarily reflect the views and policies of the Asian Development Bank (ADB), its Board of Governors, or the governments they represent. ADB does not guarantee the accuracy of the data in any documents and materials posted on this website and accepts no responsibility for any consequence of their use. By making any designation of or reference to a particular territory or geographic area, or by using the term “country” in any documents posted on this website, ADB does not intend to make any judgments as to the legal or other status of any territory or area.
